TABLE OF CONTENTS
Introduction
If your local contract has been set up to record and manage payments, you can access and monitor payment details directly from the Contracts tab. This includes recording payments and reviewing payment dashboards to ensure accurate tracking.
The payment framework associated with your contract determines how calculations are made. There are four main payment frameworks used in Ardens Manager, each tailored to specific contract requirements. This support article will walk you through these frameworks and their key components.
Accessing Payment Features
Under the Contracts tab of your Local Contract Dashboard,
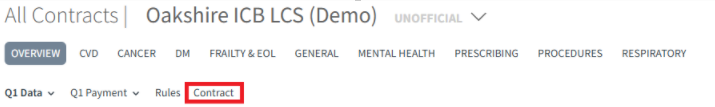
Navigate to the payment section. Here, you will see the option to Record Payment on Ardens Manager listed next to Mechanism.

Once the contract is active, you can click on the Payment tab to view the payment dashboard. This dashboard displays calculations based on the selected payment framework.
Payment Frameworks Overview
There are four payment frameworks available in Ardens Manager:
- Point Payments
- Activity Payments with Instalments
- Activity Payments
- Block Payments
Each framework has unique rules and calculations. Below is a detailed explanation of the first framework, Point Payments.
Point Payments
The most commonly used payment method is the Point Payments framework. It functions similarly to QOF (Quality and Outcomes Framework) and NCD (Network Contract DES) payments. Payment is calculated using a specific formula, which may vary depending on the contract.

- Point Value: For local contracts, the point value is typically based on the average practice list size of the commissioning group. However, commissioners can set this to any value.
- Provider Register: Provider registers are updated monthly using data extracted from the NHS Digital website.
- Average Provider Register: This is the average list size across the commissioning group.
- Provider Disease or Indicator Count: Contracts specify whether disease prevalence or indicator prevalence is used to weight payment calculations.
- Disease Prevalence: Payments are weighted based on your practice's prevalence for specific conditions. If no national disease prevalence is entered, no weighting is applied.
- Indicator Prevalence: Each indicator has its own specific prevalence used for weighting.
If your practice list size matches the average provider register (11,934), you will receive 1p per registered patient for every point achieved.
Activity Payments with Instalments
This framework is based on activity payment, with the predicted instalments made monthly or quarterly. Payments can be adjusted manually.
Activity Payments
This framework is based on activity payment. Payments are made monthly, quarterly or annually.
Block Payments
This framework is based on monthly, quarterly or annual payments.
If you require any further assistance on the process above, please contact the Ardens Manager Support Team at support-manager@ardens.org.uk
